The Tool Box
Health Care
The League of Extraordinary Providers
Harm Reduction
Elimination Tools
Hepatitis Treatment Guidelines
Additional Resources
Oregon Viral Hepatitis Collective
The Oregon Viral Hepatitis Annual Meeting

Oregon Viral Hepatitis Elimination Plan
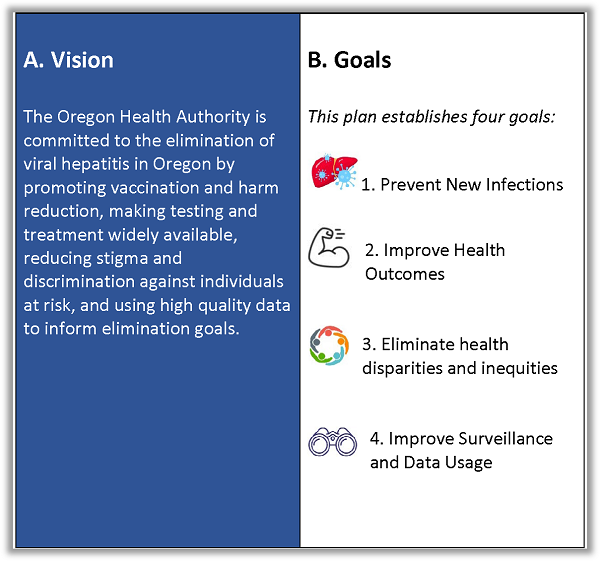 The Oregon Viral Hepatitis Program has developed a draft viral hepatitis elimination plan based on input obtained from Oregon’s Viral Hepatitis Collective.
The Oregon Viral Hepatitis Program has developed a draft viral hepatitis elimination plan based on input obtained from Oregon’s Viral Hepatitis Collective.
Goals
Our four overarching goals align with national objectives and match goals identified by Oregon’s Viral Hepatitis Collective, which completed a statewide viral hepatitis planning process in 2016.
Objectives
Objectives focus on key outcomes and key process points and are outlined for each overarching goal.
Strategies
Strategies suggest ways to meet objectives and can be measured to ensure that we stay on track to meeting our goals by 2030.
